There is increasing evidence that neuroinflammation plays a role in various neurodegenerative diseases like Alzheimer’s, Dementia or Parkinson’s. This newsletter aims to explain what neurodegenerative conditions are, how they develop and which risk factors to consider. Additionally, we’ll explore the action steps at Paracelsus.
What are neurodegenerative diseases?
The brain is composed of a vast network of nerves interconnected through synapses. These synapses have receptor sites, where neurotransmitters are transmitted through very short pathways.
In the case of Parkinson’s, for instance, it is the receptors for dopamine situated in a specific area of the substantia nigra (black substance) that undergo degeneration due to deposits of misfolded proteins (Alpha-synuclein=Lewy bodies), a process not yet fully understood. Besides this specific process, many other occurrences take place throughout the body even before the onset of the disease, collectively referred to as a Multi-System Disorder. This involves disruptions in smell, sensation, mood, the autonomic nervous system, sleep, gastrointestinal tract, and more. For example, chronic constipation is often associated with Parkinson’s decades before its manifestation (1).
A similar scenario unfolds in Alzheimer’s dementia, where particularly tau proteins accumulate on nerves, leading to the destruction of significant areas of the brain (refer to Figure 1). While only few are genetically determined, there is evidence of some genetic risk factors, such as the Apolipoprotein E in Alzheimer’s, believed to shield nerves from harmful substances.
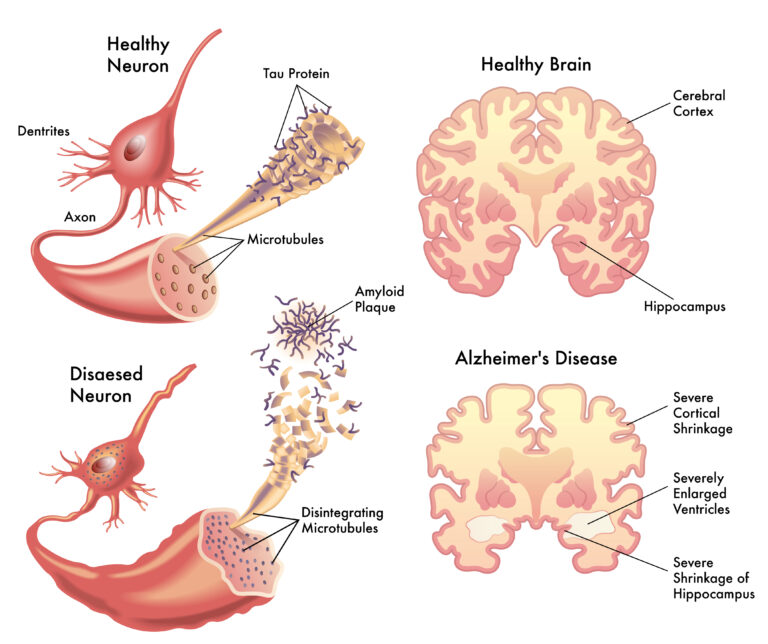
Figure 1: In Alzheimer’s disease, tau proteins are deposited on the nerves and destroy neurons. rob3000 – stock.adobe.com
Therapy approach in conventional medicine
For neurodegenerative diseases such as Alzheimer’s and Parkinson’s, there is currently no therapy that significantly influences the course of the conditions. In the case of Parkinson’s, there are medications like L-Dopa and Amantadine that can markedly improve symptoms such as stiffness (rigor), tremors, and slowed movements (bradykinesia) in patients with early, mild forms of the disease. Unfortunately, these medications also come with long-term side effects, leading to hesitancy in younger patients to take them.
For Alzheimer’s, even the improvement of symptoms through medication is minimal. A new drug for Alzheimer’s, Lecanemab, is currently being approved, aiming to reduce Tau proteins. However, it must be administered in very early stages to have a slightly positive impact on the progression of the disease over several years. Despite this modest success and considerable side effects, such as relatively frequently occurring brain swelling, health insurances and patients are provided with therapy costs exceeding 25,000 CHF annually.
Prevention and intervention in neurodegenerative disease
Fortunately, the outlook for preventive measures is considerably better. As the initial symptoms of neurodegenerative diseases may precede their onset by decades, there are ample warning signs to initiate preventative measures in a timely manner. According to official statistics, the following highly effective measures can prevent 40% of dementia cases, as illustrated in Figure 2 (2). We at Paracelsus believe that a better understanding of the root causes could significantly increase this percentage. Even in more advanced early stages of the diseases, therapies and preventive measures remain highly effective, although their efficacy tends to diminish in progressive stages.
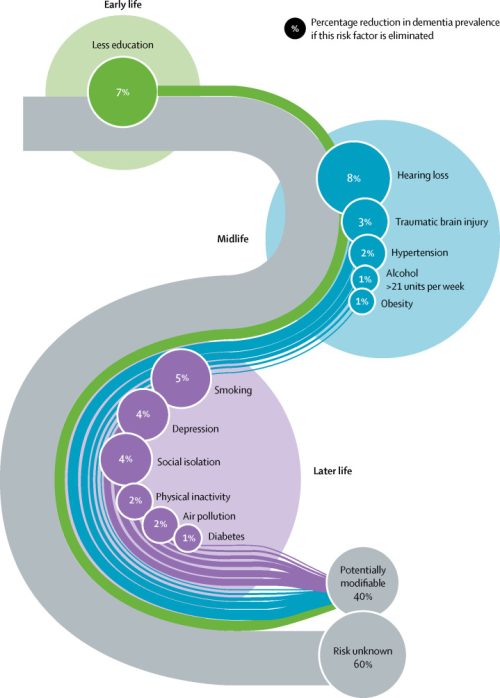
Figure 2: Dementia prevention, intervention and care.
Livingston, Gill, et al. “Dementia prevention, intervention, and care: 2020 report of the Lancet Commission.” The Lancet 396.10248 (2020): 413-446.
Cause-orientated approach
In our clinic, we have extensively observed many cases of neurodegenerative disease over the years, uncovering additional important factors that could significantly influence the course of these conditions. This individualized investigation into the causes for each patient is of great importance as it assists us in developing better treatments. In addition, understanding the multicausality of neurogenerative disease is a crucial step towards more effective preventive measures. The identification of these factors contributes to improving the quality of life and most importantly to slowing the progression of these debilitating diseases.
The most important factors, which we consider and start searching for in each individual patient suffering for example of Parkinson’s or Alzheimer’s:
– Environmental toxins, especially heavy metals
– Neurotoxins
– Electromagnetic fields (EMF), especially in the bedroom
– Nutritional deficiencies and malpractices
– Lifestyle factors like exercise, sleep, breathing etc.
– Emotional wellbeing / Body Mind issues
– Dental Health
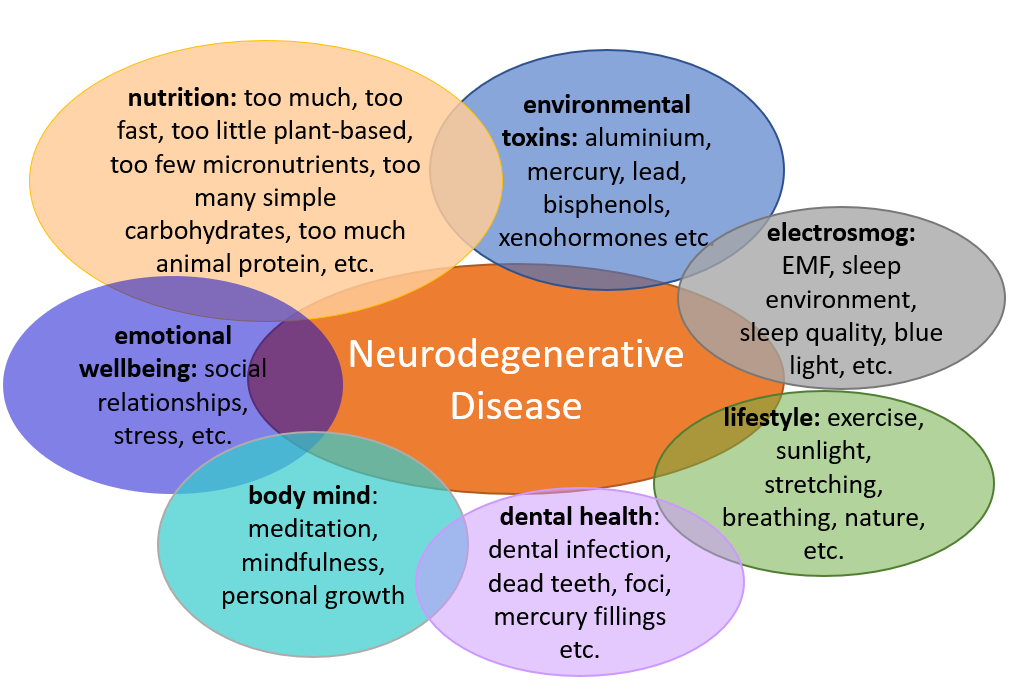
Figure 3: Biological Medicine identified factors associated with neurodegenerative disease
Therapy approach for neurodegenerative diseases in biological medicine
Pillar 1: Detoxification
After careful diagnosis and root cause analysis, we usually find a toxic load of heavy metals or other environmental toxins such as bisphenols etc. The Paracelsus Clinic specializes in detoxifying the body with various therapeutic measures, e.g. we can specifically detoxify heavy metals with chelate infusions.
Plasma Apheresis for specialized detoxification
Since this year we also offer a plasma cleaning method called Plasma-Apheresis at Paracelsus (for more info see Newsletter). The goal of plasma apheresis is to remove disease-causing substances, such as inflammatory factors triggering neuroinflammation, while retaining the beneficial components. Although randomized controlled studies are still pending, this procedure is already being applied for neurodegenerative diseases, with reported positive effects in individual cases. However, it should be noted that the therapy likely needs to be performed on a regular basis as long as the root-causes are not addressed.
Holistic Dental Medicine
For optimal detoxification, Paracelsus dentistry holds significant importance for us. Our longstanding collaboration with the Paracelsus Dental Clinic has proven to be highly impactful for our patients. Individuals with neurodegenerative diseases are advised through dental tomography and toxicological examinations to explore the possibility of a dental condition triggering the illness. It is noteworthy how frequently dental and heavy metal loads accompany neurodegenerative diseases and can directly influence the course of the disease positively after proper dental restoration.
Our observations are supported by numerous scientific studies, indicating that heavy metals such as mercury from amalgam fillings can play a significant role in neurodegenerative diseases like Alzheimer’s (3-6). However, the removal of amalgam should be conducted with maximum protective measures and extreme caution. This approach has been successfully practiced for many years at Paracelsus Dental and has proven its medical efficacy in many cases. Therefore, we cannot emphasize enough how crucial it is to consider dental health, especially when chronic diseases are involved.
Pillar 2: Microbiome and gut-brain axis
The microbiome, the community of bacteria and other microorganisms in the digestive tract, influences not only digestion but also the immune system, the nervous system and inflammatory responses in the body. Fortunately, the focus on the microbiome has gradually grown in conventional medicine the last years, something that Biological Medicine has been observing, studying, and successfully treating for many decades. Especially in neurodegenerative disease the microbiome is thought to play an important role in influencing neuroinflammation (7,8).
The connection between the microbiome and the nervous system is described by the term “gut-brain axis” and involves various mechanisms in neurodegenerative disease (see Figure 4):
- Firstly, beneficial substances such as short-chain fatty acids or neurotransmitters like dopamine are produced by “good” gut bacteria and transmitted directly to the brain through the blood and lymph.
- Additionally, certain harmful substances like biofilm proteins or deposits typical of Parkinson’s (Lewy bodies) are produced by “bad “gut bacteria and transported directly to the brain via the vagus nerve.
- In cases where various substances pass through the intestinal wall (particularly pronounced in “leaky gut”), inflammatory substances excreted by “bad” bacteria are released into the blood, causing neuroinflammation. This, in turn, leads to increased deposition of harmful substances such as tau proteins. These substances also contribute to the blood-brain barrier, which protects the brain, becoming porous, resulting in a kind of “leaky brain” (7,8).
From "leaky gut" to "leaky brain"
One of the primary causes of neuroinflammation and diseases such as dementia, Alzheimer’s, autism, MS, and depression is increasingly found to be in the intestinal tract according to a growing body of research (8). The Paracelsus Clinic has accumulated decades of experience in gut restoration. We start the process with a comprehensive stool test. Utilizing detailed microbiome diagnostics, we can customize the gut restoration therapy plan and administer targeted probiotics (beneficial gut bacteria) and prebiotics (specific fibres promoting beneficial gut bacteria). Particularly in neurological diseases, we often find inflammation of the intestinal mucosa which can lead to the Leaky Gut Syndrome. As described above, Leaky Gut is correlated with Leaky Brain and thus we put special focus on healing the gastro-intestinal mucosa.
The therapeutic approach at Paracelsus, similar to the study mentioned in Figure 4 (9), comprises four essential components:
- Pre- and probiotics to establish a healthy gut flora.
- Diet and supplements that can modify the microbiome to create an optimal environment for beneficial bacteria.
- Colon hydrotherapies with re-floridation.
- Restoration of the intestinal mucosa to diminish gut-specific neuroinflammation.
Additionally, if necessary, specialized methods such as the Paracelsus Intestinal Biofilm and Parasite Cleanse or the Liver Detoxification Program are employed to rebuild gut health from the ground up. This approach enables us to achieve long-term success.
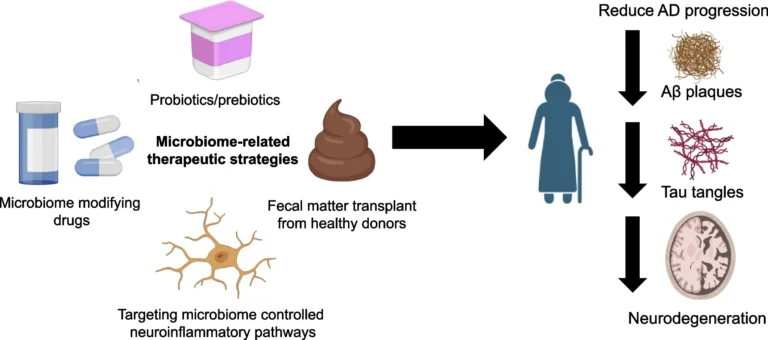
Figure 4: Microbiome restauration to reduce neurodegeneration in Alzheimer’s
Chandra S. et al. The gut microbiome in Alzheimer’s disease: what we know and what remains to be explored. Mol Neurodegeneration 2023: 18: 9
Pillar 3: Regeneration
In today’s modern and stressful world, holistic regeneration therapy is gaining increasing significance, particularly in the context of neurodegenerative diseases. Our therapeutic approach not only considers symptomatic treatment but encompasses the body, mind, and soul. As brain inflammation plays a central role in the development and progression of neurodegenerative diseases such as Alzheimer’s, the reduction of neuroinflammation through targeted remedies is essential.
At the Paracelsus Clinic depending on identified root causes, our treatment integrates the following (as an example):
- Biological anti-inflammatory therapies, such as frankincense treatments (Boswellia Serrata), procaine, correction of patients’ fatty acid profiles etc. Pulsed electromagnetic field therapy can also work well in cases of excessive inflammation.
- Neural therapies with remedies from Sanum, anthroposophic medicines, and homeopathics applied to specific acupuncture points can alleviate energy blockages and strengthen the autonomic nervous system (closely linked to the gut) (see Figure 4).
- Orthomolecular therapies with trace elements, vitamins, and specific fatty acids.
- Phytotherapy and Nutritional therapy
Examples of Supplements that play a role
There are several natural remedies that particularly support the nervous system and can regenerate nerve cells.
Omega-3 fatty acids
Omega-3 fatty acids play a crucial role in the health of the nervous system and generally exhibit anti-inflammatory effects. Of particular importance are the two Omega-3 fatty acids, Eicosapentaenoic Acid (EPA) and Docosahexaenoic Acid (DHA).
DHA is a major component of cell membranes in the brain and nerve cells, influencing cell structure and function. It is essential for neural communication, signal transmission between nerve cells, and overall brain function. Omega-3 fatty acids, especially EPA, also exhibit anti-inflammatory properties. Since, as explained above, inflammation in the body, including neuroinflammation in the brain, plays a crucial role in the onset and progression of neurodegenerative diseases, the intake of Omega-3 fatty acids can thus help modulate and alleviate these inflammatory processes. This may positively impact the course of diseases like Alzheimer’s.
However, as some individuals struggle to efficiently convert Omega-3 fatty acids from plant sources such as flaxseed oil and hemp oil into biologically active forms, alternative sources should be considered.
Algal oil, derived from algae, offers a particularly recommendable alternative. Algae are the primary source of Omega-3 fatty acids in the food chain for fish. Therefore, algal oil provides a direct and sustainable way to consume essential Omega-3 fatty acids, especially EPA and DHA, without relying on fish consumption. This approach is not only attractive from a health perspective but also from environmental, toxicological, and ethical standpoints, as fish are becoming increasingly scarce and heavily burdened by environmental toxins.
Vitamin D
Vitamin D plays a crucial role in the health of the nervous system, and there is evidence suggesting that a deficiency in Vitamin D could be linked to neurodegenerative diseases such as Alzheimer’s (10-12).
In the brain, Vitamin D influences the production of neurotrophins, proteins that promote the survival and growth of nerve cells. Vitamin D also possesses anti-inflammatory properties and may contribute to reducing neuroinflammation in Alzheimer’s. Additionally, Vitamin D can protect against oxidative stress. Oxidative stress occurs when the body lacks antioxidants, allowing harmful free radicals to damage cells. Protection against oxidative stress will slow the aging process and protect against neurodegenerative diseases.
Due to the reduced exposure of unprotected skin to sunlight nowadays, paradoxically resulting even in more sunburns without the natural build-up of skin protection, most people have insufficient Vitamin D formation. Therefore, Vitamin D supplementation is unavoidable in the majority of cases.
4. Pillar: Autonomic Nervous System
The autonomic nervous system (ANS) is responsible for regulating bodily functions that are not consciously controlled, such as heart rate, blood pressure, and digestion. As described above, in neurodegenerative diseases, the ANS can be impaired, leading to dysregulations in the brain (see Figure 4).
The connection between neurodegenerative diseases, the ANS, sleep, and the microbiome is a complex and continually evolving research area. In our therapeutic approach, we are very interested in understanding how these factors interrelate and how Body-Mind therapies could exert a positive influence.
In patients with neurodegenerative diseases we often observe that sleep is significantly disrupted. Interestingly, there is also a reciprocal relationship between sleep and the microbiome – disturbed sleep leads to a disrupted microbiome, and conversely, a disturbed microbiome can result in disrupted sleep.
Given the close connection between the autonomic nervous system, the enteric (gut) nervous system and the brain, it is easy to understand that an imbalance in the microbiome (dysbiosis) and/or imbalance of the ANS may be associated with a dysfunction of brain nerves (8,9). Thus, the disrupted gut-brain axis can potentially be regulated through body-mind therapies, accompanied by an intensive gut restoration.
Body Mind Therapies at Paracelsus
At the Paracelsus Clinic, we provide Psycho-Kinesiology, specialized training in Mind-Body Medicine (MBM), and Mind-Body-Stress-Reduction (MBSR) to break this vicious cycle. Paracelsus Body-Mind Therapies address the connection between the body and mind, contributing to stress reduction, balancing the ANS, and improving sleep. By promoting relaxation and mindfulness, Body-Mind Therapies can indirectly have positive effects on the microbiome and modulate inflammatory processes (13).
In summary, considering Biological Medicine in the context of neurodegenerative diseases like Alzheimer’s reveals that addressing underlying causes can yield promising results. Targeting the reduction of neuroinflammation and restoring a healthy microbiome opens new avenues for the therapy and prevention of these complex diseases. Analysing the interaction between the environment, the body and the mind, Biological Medicine offers not only to alleviate symptoms but also to modulate underlying processes, to get to the root of neurodegenerative diseases.
For optimal detoxification, Paracelsus dentistry holds significant importance for us. Our longstanding collaboration with the Paracelsus Dental Clinic has proven to be highly impactful for our patients. Individuals with neurodegenerative diseases are advised through dental tomography and toxicological examinations to explore the possibility of a dental condition triggering the illness. It is noteworthy how frequently dental and heavy metal loads accompany neurodegenerative diseases and can directly influence the course of the disease positively after proper dental restoration.
References:
1. Drobny A et al. Molecular Communication Between Neuronal Networks and Intestinal Epithelial Cells in Gut Inflammation and Parkinson’s Disease. Front Med (Lausanne) 2021; 8:655123.
2. Livingston G. et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. The Lancet 2020; 10248:413-446.
3. Mutter J. et al. Alzheimer disease: mercury as pathogenetic factor and apolipoprotein E as a moderator. Neuroendocrinology Letters 2004; 25.5: 331-339.
4. Mutter J., Naumann J., Schneider R., Walach H. Quecksilber und Alzheimer-erkrankung. Fortschritte der Neurologie· Psychiatrie 2007; 75(09):528-538.
5. Mutter J. et al. Does inorganic mercury play a role in Alzheimer’s disease? A systematic review and an integrated molecular mechanism. J of Alzheimer’s Dis 2010; 22.2:357-374.
6. Siblerud R., Mutter J., Naumann J. et al. A hypothesis and evidence that mercury may be an etiological factor in Alzheimer’s disease. Int. J of Environ Res and Pub Health 2019; 16.24:5152.
7. Obrenovich MEM. Leaky Gut, Leaky Brain? Microorganisms. 2018; 6(4):107.
8. Elfil M. et al. Implications of the gut microbiome in Parkinson’s disease. Movement Disorders 2020; 35.6 :921-933.
9. Chandra S. et al. The gut microbiome in Alzheimer’s disease: what we know and what remains to be explored. Mol Neurodegeneration 2023; 18:9.
10. Shen L, Ji HF. Vitamin D deficiency is associated with increased risk of Alzheimer’s disease and dementia: evidence from meta-analysis. Nutr J. 2015; 14:76.
11. Annweiler C, Llewellyn DJ, Beauchet O. Low serum vitamin D concentrations in Alzheimer’s disease: a systematic review and meta-analysis. J Alzheimers Dis. 2013;33(3):659-74
12. Balion C et al. Vitamin D, cognition, and dementia: a systematic review and meta-analysis. Neurology. 2012; 79(13):1397-405.
13. Fox KC et al. Is meditation associated with altered brain structure? A systematic review and meta-analysis of morphometric neuroimaging in meditation practitioners. Neurosci Biobehav Rev. 2014; 43:48-73.