Headaches are one of the most common reasons people seek medical attention, occurring either episodically or chronically (1). They can be triggered by various factors such as stress, smoking, hunger, quality of sleep, specific foods (like chocolate, cheese, and alcohol), hormones, and weather conditions etc. (2). Typically, individuals consult a doctor when headaches become particularly severe, persistent, or unresponsive to over-the-counter pain relievers. At this point, it becomes crucial for us to identify the underlying causes.
Different types of headaches
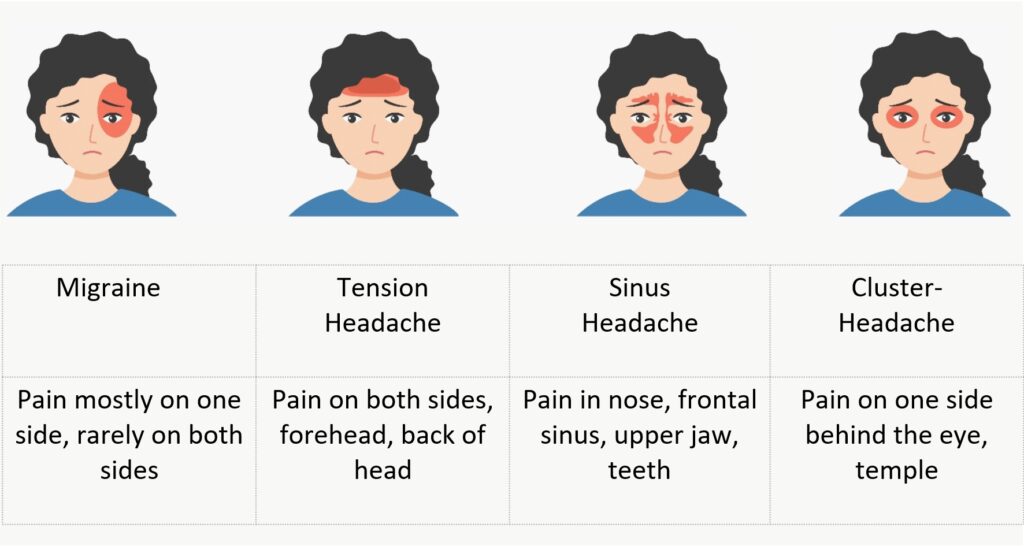
Migraine: Big Impact on Quality of Life
The second most reported pain in the head is migraine, which often poses a massive burden on the patient’s quality of life. A migraine is quite different from a normal headache, which almost everyone has from time to time. A migraine attack is characterized by a sudden onset of sharp, stabbing pain, usually on one side of the head only. They are much more severe than normal headaches and are usually accompanied by other symptoms such as visual disturbances, nausea, etc. Persistent migraine episodes often lead to mixed symptoms of chronic migraine and tension headaches. Chronic headaches are defined as headaches lasting at least 15 days a month or more than 4 hours a day for three months. Women are more frequently affected, with the highest incidence occurring in the middle decades of life (around the age of 40) (3).
Tension Headaches: Collaboration with Dental Department Inevitably
Tension headaches are the most common headache disorder and is characterized by a dull, pressure pain which usually radiates throughout the entire head. The pathophysiology of tension-type headaches is still inadequately understood. Increased tension of the neck muscles, jaw tension and associated irritation of the nervous system are discussed as potential causes (4).
Conventional mainstream medicine treats tension-type headaches pharmacologically with analgesics such as amitriptyline or NSAIDs like ibuprofen. However, regular intake of such pain medications can lead to a condition known as “medication-overuse headache.” Pain can be triggered by both hypersensitivity to the active ingredient and by overdose or withdrawal. Often, after discontinuing long-term treatment with analgesics, this medication-overuse headache occurs. Since satisfactory therapeutic results are usually not achieved with the use of conventional medicine, a significant proportion of patients seek complementary therapeutic approaches.
In case of tension headaches, we always collaborate with the Paracelsus Dental department. There is a condition called Temporomandibular Joint (TMJ) Dysfunction which is often associated with jaw tension and headaches. The TMJ connects your jaw to the skull, and issues in this joint can cause pain that radiates to the head (5).
It is also possible that overactivity or tension in the jaw muscles caused by clenching or grinding teeth (bruxism), can lead to headaches. Furthermore, poor dental alignment, known as malocclusion, can cause stress on the jaw muscles and contribute to headaches. And lastly, even tooth problems like cavities, infections, or other dental issues may lead to referred pain, causing headaches. Thus, effective management often involves collaboration between dentists, osteopaths, and medical staff to address the various aspects contributing to jaw tension and headaches.
Sinus Headache: Understanding Allergies for Effective Relief
The sinus headache, often caused by swelling of the nasal sinuses, allergies, or chronic sinusitis, is classically characterized by headache focused on the frontal area. Typically, symptoms worsen when the head is tilted forward. Patients frequently experience additional symptoms such as seasonal allergy-related issues, sinus-bronchial syndrome, fatigue, etc. Moreover, these symptoms may also be associated with a dental focus, indicating dental involvement.
The evaluation of this sinus headache again requires interdisciplinary collaboration with the dental clinic and can be detected through imaging (ultrasound or CBCT diagnostics).
Cluster Headaches: Episodic and Chronic
Cluster headaches are intense one-sided attacks of head and facial pain typically lasting between 15 and 180 minutes if left untreated. The primary pain is located behind the eyes and in the forehead and temple regions. To be classified as cluster headache, a minimum of 5 attacks with at least one additional symptom (conjunctival redness, tearing, nasal congestion, runny nose, pupil constriction, drooping eyelid, eyelid swelling, sweating on the forehead and face) need to be defined. Episodic and chronic cluster headaches are distinguished, with the majority suffering from chronic episodes. Attacks often occur regularly at the same time of day, often after falling asleep or in the early morning.
Considering the root cause, it is crucial to maintain a ‘holistic perspective’ on the patient and for the treatment plan it is important to take into account the multifactorial factors involved such as allergies, dental status, posture, nutrition and stress regulation.
Detailed Headache Diagnosis for the Best Treatment Strategy
The diagnosis of headaches is often determined based on the patient’s medical history. It is crucial to maintain detailed documentation to understand the duration of headache attacks and associated symptoms. We inquire about specific triggers, therapeutic measures, and past treatments for attacks and for prevention and assessing their effectiveness. Keeping a headache diary provides valuable information to the doctor during the initial contact, helping recognize patterns and potential triggers, such as tyramine in wine and cheese, nitrites in processed meats, caffeine, glutamate, etc. These vasoactive substances and other everyday toxins need to be identified. In our experience at Paracelsus, colon hydrotherapies provide immediate relief in this regard.
Certain primary headache disorders, like migraines, have a familial tendency, making information about family headache history important. Physical and neurological examinations also form a crucial basis for diagnosis. In some cases, additional investigations may be conducted, such as craniosacral and spinal assessments, dark-field microscopy, laboratory tests, heavy metal exposure measurement, stool analysis, dental assessment, or imaging (e.g., DVT, ultrasound, CT, or MRI of the brain). For most headache disorders, magnetic resonance imaging (MRI) of the skull is preferred due to its high resolution and lack of radiation exposure. In emergency situations or specific circumstances, computed tomography (CT) may also be used.
Biological-Integrative Treatment Approach
After completing the diagnostic procedures and identifying the possible causes, a holistic treatment plan can be established. Biological Medicine can offer many successful treatment modalities for most types of headaches and their different aetiologies.
Neural therapy, in particular, is an effective method for treating headaches, pain in general and various other diseases. By injecting small amounts of procaine (local anesthetic) combined with homeopathic remedies, regulatory blockages can be removed and thus initiating regulation and self-healing processes.
How does procaine work, and why is an anaesthetic necessary? In the 1920s, the Huneke brothers discovered a way to use local anaesthetics not only for local anaesthesia but also for therapy. The “Neural Therapy according to Huneke” thus developed, can be used for eliminating energy blockages in tissues. A healthy organism can compensate for minor dysfunctions by self-regulating which requires unimpeded information exchange. Neural therapy is considered as a regulatory therapy, re-establishing optimal tissue regulation, similar to acupuncture and is widely accepted scientifically. Applying neural therapy to an interference field, will often stop the pain in other parts of the body immediately. The interference filed or foci is the point from which the pain originates, such as encapsulated bacterial colonies in dental cavities or chronic inflammation. If the patient is symptom-free immediately after the injection of the local anaesthetic, the foci has been successfully identified, and the body is animated to self-regulate while the anaesthesia “relaxes” the foci point. This reset impulse is often enough for self-healing to occur.

Headache Relief Through Nutrition
The nutritional approach to alleviating headaches has been extensively researched, with plant-based nutrition yielding the best results.
In a study, the group following a plant-based diet demonstrated a significant reduction in headache severity compared to a placebo group (6). Saturated fats found mainly in animal products such as dairy and meat had the most significant negative impact. Reducing dietary fat to less than 30 grams per day led to a six-fold decrease in the frequency and intensity of headaches (7,8).
Even a moderately low-fat diet (less than 20% fat) showed significant decreases in headache frequency and severity. This suggests that reducing the intake of saturated fats, primarily found in meat, processed food and dairy products, may help control migraine attacks (9,10). In contrast green vegetables, rich in magnesium and other valuable compounds, could play a role in reducing headaches. Since magnesium supplements often cause diarrhoea, vegetable sources of magnesium are often preferred (11,12). It is advisable to include magnesium-rich foods such as green leafy vegetables, beans, nuts, seeds, and whole grains in the diet. At Paracelsus we also offer magnesium infusions to replenish the body with magnesium if needed.

Unlocking Relief: A comprehensive approach at Paracelsus
Alongside neural therapy and nutritional therapy, physical therapies like local hyperthermia (heat treatments), manual fascia or deep tissue massages, cupping, ion-induction therapy (Papimi) or Magnetic Field Therapy are considered. In addition, orthomolecular methods (like procaine, magnesium, mineral infusions), targeted phytotherapy and homeopathic remedies have proven effective and act therapeutically to significantly reduce the frequency and intensity of attacks (13). Traditional Chinese medicine (TCM) and acupuncture are also used in conjunction with neural therapy. At the Paracelsus Clinic, patients are always individually assessed, and accordingly, a treatment plan is created.
Balancing Lifestyle for Pain Relief
Mind Body Medicine aims to support individuals in developing a health-promoting lifestyle in their daily lives (14). Special attention is given to the influence of emotional stress, mind sets, breathing, body posture and behaviour which could influence pain episodes (15).
The roots of Mind Body Medicine lie, among other things, in the findings of stress research, supporting individuals in developing and maintaining the ability for self-care. Mind Body medicine can also provide guidance in finding meaning in one’s own life and current life situation. Thus, in addition to conventional and naturopathic medicine, Mind Body Medicine offers a resource-oriented therapeutic approach that empowers the patient to actively participate in their own recovery and health maintenance. Identifying stressors and triggers has proven to be very successful for treating tension headaches. Stress management through mindfulness (Mindfulness-Based Stress Reduction Program – MBSR), movement therapy, meditation, biofeedback, kinesiology, progressive muscle relaxation, hydrotherapy, and other therapies can be beneficial (15). For migraine patients, it is also crucial to pay attention to sleep quality, daily routines, and abstaining from toxic substances (e.g. additives, alcohol, and smoking). In some cases, an initial complex inpatient multimodal therapy intervention may be advisable.
Overall, there is a growing interest in Biological Medicine and a holistic approach in treating headaches. Instead of just alleviating symptoms by administering pain medication, Biological Medicine focuses on investigating the causes and aims to identify the underlying triggers. Through a comprehensive analysis of the medical history, headache diaries, and diagnostic procedures, individualized therapy plans can be developed, incorporating both conventional and complementary approaches. Our short-term goal is to find a combination of methods that lead to successful reduction in attack frequency and intensity. Our enduring objective for individuals with chronic headaches is to consistently unlock pain relief, promote self-healing, and enhance overall quality of life.
References:
1. Ha H, Gonzalez A. Migraine Headache Prophylaxis. Am Fam Physician. 2019;99(1):17-24.
2. Bega D. Complementary and Integrative Interventions for Chronic Neurologic Conditions Encountered in the Primary Care Office. Prim Care. 2017;44(2):305-322.
3. Peters GL. Migraine overview and summary of current and emerging treatment options. Am J Manag Care. 2019 Jan;25(2 Suppl):S23-S34.
4. Peck CL, Kraft GH. Electromyographic biofeedback for pain related to muscle tension. A study of tension headache, back, and jaw pain. Arch Surg. 1977 Jul;112(7):889-95.
5. Matheson EM, Fermo JD, Blackwelder RS. Temporomandibular Disorders: Rapid Evidence Review. Am Fam Physician. 2023 Jan;107(1):52-58.
6. Jain MM, Kumari N, Rai G. A novel formulation of veggies with potent anti-migraine activity. Int J Comput Biol Drug Des. 2015;8(1):54-61.
7. Hindiyeh N, Aurora SK. What the Gut Can Teach Us About Migraine. Curr Pain Headache Rep. 2015;19(7):33.
8. Bunner AE, Agarwal U, Gonzales JF, Valente F, Barnard ND. Nutrition intervention for migraine: a randomized crossover trial. J Headache Pain. 2014;15:69.
9. Bic Z, Blix GG, Hopp HP, Leslie FM, Schell MJ. The influence of a low-fat diet on incidence and severity of migraine headaches. J Womens Health Gend Based Med. 1999;8(5):623-30.
10. Ferrara LA, Pacioni D, Di fronzo V, et al. Low-lipid diet reduces frequency and severity of acute migraine attacks. Nutr Metab Cardiovasc Dis. 2015;25(4):370-5.
11. Pfaffenrath V, Wessely P, Meyer C, et al. Magnesium in the prophylaxis of migraine–a double-blind placebo-controlled study. Cephalalgia. 1996;16(6):436-40.
12. Veronese N, Demurtas J, Pesolillo G, et al. Magnesium and health outcomes: an umbrella review of systematic reviews and meta-analyses of observational and intervention studies. Eur J Nutr. 2019;
13. Okoli GN, Rabbani R, Kashani HH, et al. Vitamins and Minerals for Migraine Prophylaxis: A Systematic Review and Meta-analysis. Can J Neurol Sci. 2019;46(2):224-233.
14. Erwin Wells R, Phillips RS, McCarthy EP. Patterns of mind-body therapies in adults with common neurological conditions. Neuroepidemiology. 2011;36(1):46-51
15. Nahman-Averbuch H et al. Identification of neural and psychophysical predictors of headache reduction after cognitive behavioral therapy in adolescents with migraine. Pain. 2021 Feb 1;162(2):372-381.




