Did you know that around one in four adults in Switzerland and Germany suffers from non-alcoholic fatty liver disease (NAFLD) – often without knowing it (1)? Are you often tired, have problems concentrating or digestive complaints such as bloating or a feeling of pressure in your upper abdomen? These unspecific symptoms could indicate a fatty liver, which, if left untreated, increases the risk of more serious illnesses such as liver inflammation, fibrosis or cirrhosis. But as the saying goes: “The liver grows with its tasks.” This proverb reflects the liver’s impressive adaptability but also its ability to regenerate and underlines how crucial timely support is for its health.
Inhalt
How does a fatty liver develop?
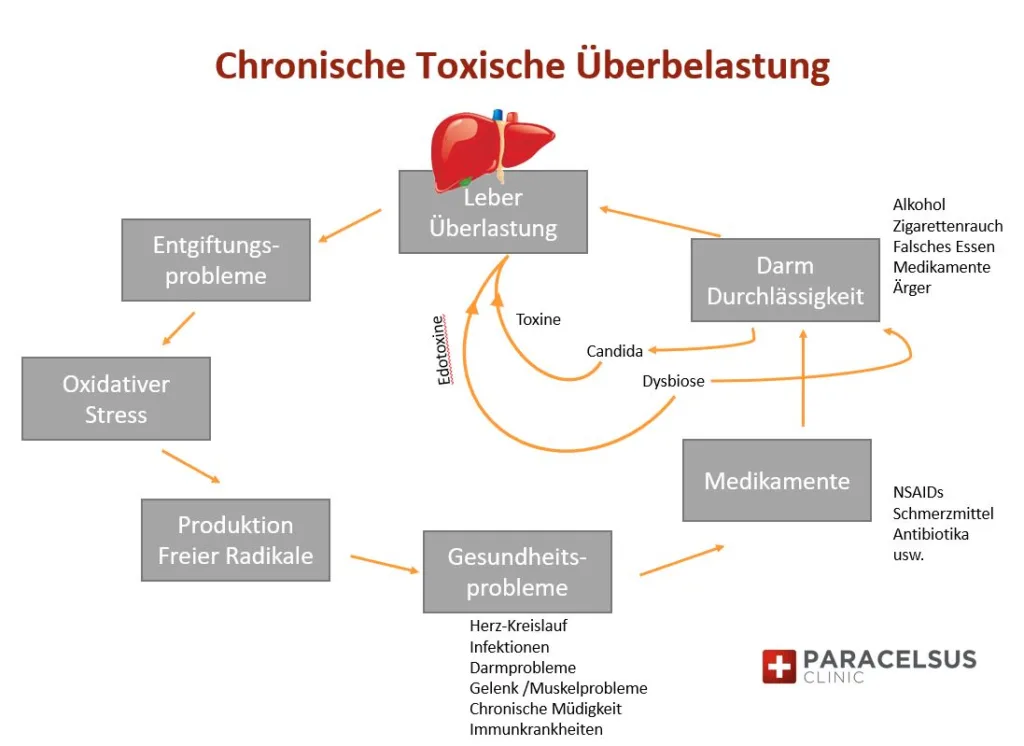
A fatty liver can be described as a chronic overload of the liver, which leads to the liver storing fat in its cells. This overload is often caused by factors such as metabolic disorders, an unhealthy diet, obesity and toxic influences such as alcohol or environmental toxins. If the liver permanently stores too much fat, this leads to fat deposits in the liver cells, resulting in poor liver function and possible damage. Fatty liver is often the first step towards serious diseases such as inflammatory fatty liver disease (NASH), liver cirrhosis or even liver cancer (2). It is therefore important to take early action to maintain and support liver health.
Non-alcoholic fatty liver disease (NAFLD)
Non-alcoholic fatty liver disease (NAFLD) encompasses a broad spectrum of conditions ranging from the accumulation of fat in liver cells (steatosis) to fibrosis (scarring). NAFLD is closely associated with metabolic disorders such as obesity, insulin resistance and elevated leptin levels (a hormone that regulates hunger and satiety). These factors promote the excessive storage of fats, especially triglycerides, in the liver cells and trigger a vicious circle. An increasing toxin load, combined with inflammation, further worsens liver function (3). The central role of the liver in metabolic and detoxification processes illustrates how crucial its health is for the overall well-being of the body.
But what exactly does this organ do and why is it so important to protect it?
Functions of the liver
The liver is often referred to as the “chemical factory of the body” – an impressive organ that works tirelessly to maintain vital processes. Its central role goes far beyond mere detoxification and includes essential functions for metabolism, the immune system and the maintenance of general body homeostasis (balance and maintenance of bodily functions such as blood pH, body temperature, blood sugar etc.). Excess glucose is stored in the liver as glycogen and released again when required to stabilize the body’s energy balance. In addition, the liver produces important fats such as cholesterol and triglycerides as well as proteins that are essential for fluid balance and the transportation of substances in the blood, such as albumin.
Particularly noteworthy is the daily production of 800 to 1000 milliliters of bile, a golden fluid that is essential for the digestion of fat and the absorption of fat-soluble vitamins (A, D, E, K). At the same time, bile serves to detoxify fat-soluble harmful substances, such as xenohormones, which are increasingly being ingested unconsciously. Bile is collected in small ducts in the liver and transported via the bile duct to the duodenum, where it unfolds its valuable effect.
The versatility of the liver is demonstrated in the area of protein metabolism: it converts animal proteins into amino acids, which either serve as a source of energy or can be converted into carbohydrates and fats. This process produces the endotoxin ammonia, a toxic by-product that is converted into non-toxic urea by the liver cells. This is transported via the blood to the kidneys and finally excreted in the urine (4). (It is therefore always important to ensure healthy kidney function).
The liver also plays a key role in blood clotting. With the help of vitamin K, it produces important proteins that are essential for this process. At the same time, it is responsible for breaking down old or damaged blood cells and thus ensures the constant renewal of the blood.
The liver also acts as a storage organ for vital nutrients. It stores vitamins such as A, D and B12, minerals and trace elements such as iron and copper as well as energy reserves in the form of fat (triglycerides) and glycogen (sugar). This storage function ensures that the body can always fall back on reserves in times of deficiency.
As a detoxification center, the liver filters harmful substances such as heavy metals, alcohol and drug residues from the blood. As the old saying goes, the liver is the purifier of the blood. This important work makes the liver an indispensable support for the immune system. With the help of special Kupffer cells, it monitors the blood flowing into the liver and removes pathogens and cell debris. However, excessive strain on the liver, for example due to an excessive intake of proteins or toxic substances, can impair its function.
In Traditional Chinese Medicine (TCM), the liver is regarded as the seat of life energy (“Qi”), which stands for vitality, creativity and drive. However, if we hesitate to protect the liver through a healthy lifestyle, we not only risk overloading this central organ, but also open the door to diseases that can affect our entire body. The liver deserves our attention – not just as a chemical factory, but as the key to a life of balance and energy.
Treatment options
There is currently no specific pharmacological therapy directly approved for NAFLD. Conventional treatments focus primarily on weight control medications, insulin sensitizers and lipid-lowering drugs. However, commonly used drugs such as GLP-1 agonists, thiazolidinediones and statins can have significant side effects, including gastrointestinal symptoms such as diarrhea, muscle pain, uncontrolled fat secretions and increased cardiovascular risk (5-7).
In contrast, we take a cause-oriented approach that addresses root problems such as toxic load, unhealthy lifestyle, gut health and nutrient deficiencies. Our focus is on sustainable lifestyle changes, personalized nutritional plans and targeted therapies that restore metabolic balance and optimize liver health.
Treatment approach of the Paracelsus Clinic
A doctor can diagnose a fatty liver through blood tests (e.g. elevated liver values such as ALT, AST, GGT), ultrasound or other diagnostic procedures. For patients who do not wish to take medication, our approach is suitable, which is based on root cause analysis, dietary changes, weight reduction, restoration of metabolic health, intestinal reconstruction and targeted relief of the liver. An intensive medical history, diagnosis and root cause analysis are required first. In addition to the conventional medical liver tests, we carry out holistic examinations to obtain a complete picture of the health situation. This includes current medication, digestion, well-being, abdominal palpation, tongue, nutrition, the autonomic nervous system (VNS analysis), laboratory values such as GGT, CRP etc. It should be noted here that the microbiome is often affected and contributes to the problem.
Intestines, nutrition and metabolic disorders
Gut health is closely linked to the development of fatty liver disease. A disturbed microbiome promotes the release of inflammatory molecules such as lipopolysaccharides (chemical compounds of sugar and fat) that promote insulin resistance. Excess body fat releases free fatty acids (FFAs) that overload the liver, while insulin resistance disrupts the regulation of glucose and lipids. Excess glucose is converted to fat and stored in the liver, increasing oxidative stress and inflammation (8). These metabolic disturbances not only impair liver function, but also promote general fatigue, poor concentration and a weakened immune system.
In order to investigate the metabolic and intestinal causes, we combine conventional medical tests with holistic methods. These include dark field microscopy to analyze the internal environment, hyperacidity and excess fats, homocysteine measurements, a fatty acid profile and stool tests (microbiome analysis). The latter provide information on the utilization of fats, proteins and glucose as well as on the intestinal flora, which plays a key role in inflammation and metabolic disorders. A nutritional questionnaire helps to identify individual triggers such as diet/nutrition and lifestyle.
Micronutrient deficiency and inflammatory processes
A deficiency of essential micronutrients plays a central role in the development and exacerbation of chronic inflammation, which significantly influences the progression of fatty liver disease. Nutrient-poor diets, especially low consumption of vegetables and phytochemical-rich (phytochemicals) foods, reduce the availability of anti-inflammatory substances such as polyphenols and anthocyanins, which could help to alleviate oxidative damage and inflammatory processes. In addition, a lack of vitamins and minerals/trace elements such as zinc, selenium and vitamin D weakens the liver’s antioxidant defense mechanisms, which promotes inflammation (8).
In obesity, high leptin levels amplify inflammatory signals in the liver, promote the release of cytokines such as TNF-α and IL-6 and accelerate tissue damage. These processes can lead to an exacerbation of NAFLD (non-alcoholic fatty liver disease) to NASH (non-alcoholic steatohepatitis), a condition associated with more severe liver damage and a higher risk of fibrosis (scarring) and cirrhosis (hardening) (9).
Toxic loads
The liver is often overloaded by environmental toxins, food additives and metabolic waste products. These stresses lead to oxidative stress, which damages liver cells and increases fat deposition (10). Insufficient availability of detoxification enzymes such as cytochrome P450 and antioxidant systems such as glutathione exacerbate the situation
For toxic loads, we analyze heavy metals using a chelate test as well as organic toxins such as xenohormones, pesticides and drug residues. In addition, we test viral loads, genetic predispositions for detoxification enzymes, heavy metal loads and other metabolic imbalances as well as micronutrients in the tissue using an oligo/check test. In particular, we test zinc, selenium – two important cofactors in the detoxification process – as well as B vitamins (e.g. folate, B6) and other important antioxidants. It is particularly beneficial to integrate this data with stool tests, blood markers and genetic testing of detoxification enzymes.
Treatment of NAFLD in biological medicine
1. the role of nutrition and lifestyle at the Paracelsus Clinic
In our view, nutrition is the key to liver health. Our anti-inflammatory metabolic diet reduces systemic inflammation, optimizes metabolism and supports liver regeneration. The nutritional advice aims to relieve the liver: this means less animal proteins (overproteinization), less sugar (fermentation) and no alcohol (acetaldehyde).
Oversupply of proteins (overproteinization): The liver cannot store amino acids, so excess proteins have to be broken down immediately. This produces ammonia, which the liver has to detoxify and convert into urea. If this detoxification capacity is exceeded, this not only puts a strain on the liver, but also leads to acidification of the tissue. During protein breakdown, acidic metabolic products are produced which can lower the pH value in the tissue. This latent acidification impairs cell functions and promotes inflammation, which can lead to various health problems in the long term. A balanced protein intake is therefore crucial.
Sugar overconsumption: Excessive consumption of sugar can damage the liver in various ways. Fructose, a component of household sugar, is metabolized directly in the liver. When overloaded, the liver converts fructose into fat, which can lead to a fatty liver. At the same time, sugar promotes fermentation processes in the intestine, especially if the microbiome is out of balance. This produces alcohol and other toxic metabolic products, which enter the liver via the portal vein.
This “endogenous alcohol” stresses the liver in a similar way to external alcohol consumption by promoting inflammation and oxidative damage. Impaired intestinal flora (dysbiosis) can exacerbate this effect, as pathogenic bacteria or yeasts produce more alcohol and other harmful substances. These processes increase the pressure on the liver’s detoxification function and can contribute to severe liver damage in the long term (11).
Alcohol consumption: Every drop of alcohol we consume has to be detoxified by the liver. This produces acetaldehyde as an intermediate product, a highly toxic substance that can damage cells, promote inflammation and increase the risk of diseases such as cancer. Studies that portrayed alcohol as healthy have since been refuted (12). Recent research shows that even small amounts of alcohol increase the risk of health problems such as cardiovascular disease, liver disease and certain cancers such as mouth, throat and even breast and bowel cancer. Alcohol is therefore not a health-promoting food, but a substance that should be consumed with caution.
The nutritional advice therefore tries to minimize exposure to toxins from food, various medications and the environment and advises to focus on natural, unprocessed foods.
We pay particular attention to the use of phytochemicals (secondary plant substances), vitamins, trace elements and minerals that are essential for detoxification processes, such as glutathione, folic acid, selenium and zinc. We also recommend intermittent fasting, a proven method for improving insulin sensitivity, reducing fat accumulation in the liver and promoting autophagy – a natural cellular detoxification process.
You can find more information about our nutritional philosophy and valuable tips in our July newsletter.
2. paracelsus clinic therapies
While a balanced diet already makes an important contribution to liver health, our specialized therapies offer additional support to specifically optimize liver function, promote detoxification and sustainably improve overall health:
- Neural therapy: Local injections to improve autonomic regulation and promote organ regeneration, especially of the liver.
- Indiba therapy: Local hyperthermia that stimulates cell regeneration and improves blood circulation in the liver.
- Various remedies for the liver are used individually. The biochemical remedy for the liver is potassium sulphuricum (e.g. Schüssler No. 6).
- Liver compresses: Targeted applications that promote blood circulation and stimulate detoxification in the liver.
- Special infusions: Customized intravenous infusions provide essential nutrients such as glutathione, zinc, magnesium and B vitamins to support liver detoxification phases 1 and 2.
- Colon hydrotherapy: A unique method of colon cleansing that reduces toxic load and improves blood flow to the portal vein, relieving the liver.

3. stress reduction
Chronic stress impairs the liver’s ability to regenerate, as it disrupts the autonomic nervous system and promotes inflammation. At the Paracelsus Clinic, we use guided breathing exercises to balance the autonomic nervous system. By calming the body, lowering cortisol levels and promoting parasympathetic activity, liver health is supported and overall wellbeing is improved.
4th Paracelsus liver detoxification program
With over 25 years of experience in the holistic treatment of liver diseases, we have developed a comprehensive and effective liver detoxification program that combines all proven therapies in a treatment plan individually tailored to you. This exclusive program not only promotes the regeneration of your liver, but also optimizes your long-term health. It includes:
- Nutritional therapy to treat the underlying metabolic blockages and drivers of inflammation.
- Advanced therapeutic interventions such as neural therapy, Indiba and colon hydrotherapy to support detoxification and liver repair.
- Special infusions that support all detoxification enzymes and organs.
- Special liver cleanses that deeply cleanse the liver of accumulated residues and improve the flow of bile.
These holistic interventions promote the restoration of liver function, increase energy, reduce inflammation and improve overall health.
The remarkable regenerative capacity of the liver
The liver is a very frugal organ and only draws attention to itself when it is working in the last third of its reserves. It simply does not hurt. Its problems almost always manifest themselves in long-distance effects such as tiredness, muscle pain, sadness, insomnia, nausea, etc.
And yet it has an extraordinary ability to regenerate, enabling recovery even after significant damage. Studies show that up to 70 % of the liver can regenerate within six months with the right measures (13).
When the liver functions optimally again, the whole body benefits and rewards us with it:
- More energy: An improved metabolism ensures lasting vitality.
- Mental clarity: Efficient detoxification reduces brain fog and increases cognitive performance.
- Pain relief: Better hormone regulation and less systemic inflammation reduce chronic pain.
- Higher metabolism: A healthy liver processes fats more efficiently and supports weight management.
- Stronger immune system: Improved detoxification and immune monitoring strengthen the body’s defenses.
- Balanced hormones: Optimized hormone metabolism promotes general well-being.
Supporting liver health through targeted treatments and lifestyle changes not only promotes its regeneration, but also transforms overall health and quality of life.
NAFLD is reversible – with the right combination of nutrition, detoxification and targeted therapies. By integrating an anti-inflammatory diet, biological medicine and innovative therapies, we help our patients to restore their liver health, reduce their toxic load and regain their vitality.
If you or someone you care about is looking for a holistic solution to promote liver health, contact us to learn more about our programs and therapies.
Save this article as a PDF for later. Click here for the PDF version!
References
1 Cholongitas E. et al. Epidemiology of nonalcoholic fatty liver disease in Europe: a systematic review and meta-analysis. Annals
of Gastroenterology. 2021; 34:404-414.
2. Pierantonelli I., Svegliati-Baroni G. Nonalcoholic Fatty Liver Disease: Basic Pathogenetic Mechanisms in the Progression From
NAFLD to NASH. Transplantation 2019; 103: e1-e13.
3. Chowdhury F Zaman et al. A Multidisciplinary Approach and Current Perspective of Nonalcoholic Fatty Liver Disease: A
Systematic Review. Cureus. 2022: 14.
4. Takaomi K. et al. Endotoxins and Non-Alcoholic Fatty Liver Disease. Frontiers in Endocrinology. 2021: 12.
5. Pafili K., Roden M. Nonalcoholic fatty liver disease (NAFLD) from pathogenesis to treatment concepts in humans. Molecular
Metabolism. 2020: 50.
6. Sodhi M, Rezaeianzadeh R, Kezouh A, Etminan M. Risk of Gastrointestinal Adverse Events Associated With Glucagon-Like
Peptide-1 Receptor Agonists for Weight Loss. JAMA. 2023 Nov 14;330(18):1795-1797.
7. Michalska-Kasiczak M. et al. Analysis of vitamin D levels in patients with and without statin-associated myalgia – a systematic
review and meta-analysis of 7 studies with 2420 patients. International journal of cardiology. 2015; 178:111-6.
8. Barchetta I. et al. Vitamin D and Metabolic Dysfunction-Associated Fatty Liver Disease (MAFLD): An Update. Nutrients. 2020:
12.
9. Drummer C. et al. Caspase-11 promotes high-fat diet-induced NAFLD by increasing glycolysis, OXPHOS, and pyroptosis in
macrophages. Frontiers in Immunology. 2023:14.
10. Enoch Cobbina et al. Non-alcoholic fatty liver disease (NAFLD) – pathogenesis, classification, and effect on drug metabolizing
enzymes and transporters. Drug Metabolism Reviews. 2017; 49: 197 – 211.
11. Jensen T. et al. Fructose and sugar: A major mediator of non-alcoholic fatty liver disease. J of Hep. 2018; 68(5): 1063-1075.
12. Ortolá R et al. Alcohol Consumption Patterns and Mortality Among Older Adults With Health-Related or Socioeconomic Risk
Factors. JAMA Netw Open. 2024;7(8):e2424495.
13. Yagi S et al. Liver Regeneration after Hepatectomy and Partial Liver Transplantation. Int J Mol Sci. 2020 Nov 9;21(21):8414



